Moving from What’s the matter with you? to What matters to you? – Humanising healthcare through social prescribing
Social prescribing is an approach that enables a range of stakeholders – often based in health-care and acting as health-care professionals – to connect individuals to a range of non-clinical or non-therapy services and activities in the community to empower them and to improve their mental well-being. The Arts on Prescription in the Baltic Sea Region project where the NDPHS Secretariat is a project partner is a Baltic model of social prescribing.
The exact “social prescriptions” are specific to each community and care setting. Typically services provide support in mental health, social inclusion, and financial and housing advice, and thereby offer participation in social activities promoting physical activity and/or creative self-expression. Thus, social prescribing is a holistic approach to health care, which promotes community-based integrated care and helps to de-medicalize health service provision.
The reason why social prescribing approaches are gaining momentum is because traditional primary health services like physicians and family doctors are overburdened by patient requests. Current statistics seem to indicate that many appointments for family doctors might not be related to a physiological health challenge or medical treatment but have a social or behavioural background, such as feeling lonely or socially isolated or showing symptoms of stress, anxiety, or depression. Dr. Bogdan Chiva Giurca, Clinical Lead and Global Director of the National Academy for Social Prescribing in the UK even estimates that as many as 1 in 5 of his patients seek care for social reasons (Bogdan 2023 – Social prescribing background). Most often family doctors cannot provide the right treatment or don’t have access to referring someone to a service that might better help to address the patients’ needs.
And that is essentially what social prescribing is about: In the most common model, physicians and other primary health care providers have the opportunity to refer patients to a specialised “link worker” who acts as a primary contact point both for patients and physicians and who collaborate with patients to determine and co-design the service that individuals might benefit from the most. Thereby, the link workers could be an individual or a team of social care workers, community workers, nurses, or also an organisation, such as an NGO.
One social prescribing initiative that has shown great results is “Music and motherhood”, recently presented at the WHO Europe HG in Copenhagen. The concept offers mothers suffering from postpartum depression (PPD) a singing group to which they can bring their babies and meet other mothers in the same situation. While there is no immediate remedy, the result shows that group singing can accelerate improvements in PPD symptoms. The idea has been developed in the UK by the Royal College of Music and Imperial College London, and successfully piloted in Romania, Italy and Denmark together with Cluj Cultural Centre, the Central Denmark Region under the supervision of the WHO Regional Office for Europe. For more insights read the full article Scalability of a singing-based intervention for postpartum depression in Denmark and Romania: protocol for a single-arm feasibility study.
A participant experience of the “Melodies for Mums” programme organised by the Breathe Arts Health Research organisation in London, UK.
Arts and cultural activities are becoming important components of social prescribing mechanisms, leading to a greater variety of activities and services. The Arts on Prescription (AoP) model we use in our Interreg BSR project, as one approach to social prescribing (next to for example Books, Education, Exercise or Culture on Prescription), is a non-therapy that offers participants to engage with arts and creative activities in group settings in a safe and supportive environment. By offering a space for creative flow, the participants have the potential to immerse themselves in activities that require concentration and focus. Engagement in arts activities also seems to provide opportunities for imagination, aesthetic and emotional expression, stress reduction, and improved self-esteem. By engaging in group activities, the participants can moreover develop social connections and social engagement. This means that AoP programmes have the potential to both increase the participants’ creative potential, improve mental health and social interaction and thus increase overall wellbeing.
The Arts on Prescription in the Baltic Sea Region model differs from other social prescribing or AoP approaches. Key aspects of the Baltic model are:
- it is a non-therapy programme;
- it is targeted towards people with mental health issues such as stress, anxiety, mild to moderate depression, or those at risk of developing mental health issues for instance, due to loneliness;
- the programme consists of varying arts categories (between 3-5), which means that the participants will engage with different art genres;
- it is voluntary based and not a part of the participant’s health or social pathway. As an explicit non-therapy programme, we do not include health progress reports of participants’ engagement in AoP programmes that are mirrored back to primary health-care providers, such as physicians. Our Baltic model rather aims at follow-up activities and plans for individuals and groups to ensure the continuation of arts and culture programmes and regular social interaction.
- the referrals are not only primary health care providers, such as physicians or clinical facilities. We also cooperate with social and other public service providers or offer self-referral options to people who wish to participate. By doing so, we aim to extend access to AoP programmes and offer services to people also at risk of developing conditions such as depression, stress, or anxiety.
- it is a cross-sectorial programme co-financed and implemented through an interdisciplinary collaboration between the relevant sectors such as the culture, health and social sector. This means that all key employees in the programme – including the culture and arts facilitators are being paid for their working hours and that the programme follows the recommendations from WHO, that such programmes should be financed cross sectors.
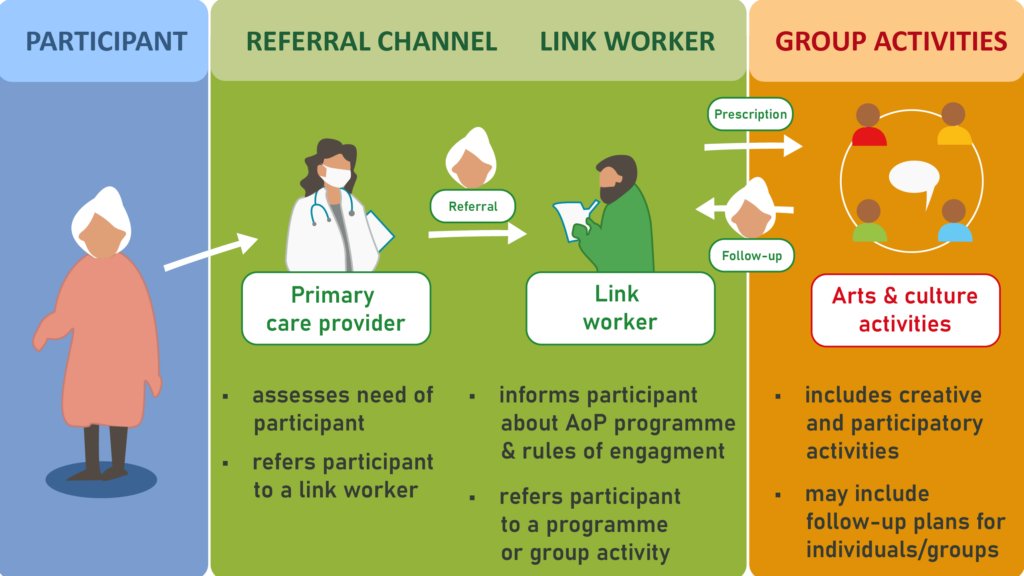
Adaptation based on WHO (2022) “A toolkit on how to implement social prescribing”
For more information on the Baltic model and the set-up of Arts on Prescription programmes visit the project page. An upcoming online practitioners’ guide will provide information and how-to-guides, fact sheets, lessons learned and audiovisual guidance for link workers, culture and arts facilitators, and decision-makers on various aspects Arts on Prescription programme.
Further reading:
- Giurca, Bogdan C. 2023 – Rethinking medicine through personalised care and social prescribing. Presentation at WHO multi-stakeholder meeting, Brussels 6. October 2023.
- National Academy for Social Prescribing and Global Social Prescribing Network.
- Jameel Arts & Health Lab.
- WHO 2022 – A toolkit on how to implement social prescribing.
Arts on Prescription receives financial support from the Interreg Baltic Sea Region and is co-funded by the European Union.
